Introduction
Cancer affects people of all ages, but is especially prevalent in older patients.1 Cancer is a leading cause of death worldwide, accounting for about one in six deaths globally.2 According to the World Health Organization (WHO), approximately 9.6 million people died from cancer in 2018 alone.1
Among many types of cancer, breast, lung, colorectal and prostate cancers are the most common types.3 The most frequent risk factors for developing cancer are family history, smoking habits and diet. However, with currently increasing life expectancy worldwide, increasing age is becoming one of the biggest risk factors. In fact, according to the National Cancer Institute, about 77% of all cancers are diagnosed in adults aged 55 or more.4 Although more than 60% of cancer patients are older than 65 years,4 no clear guidelines exist on the implementation of care for older adults in the routine daily practice in Switzerland. The optimal treatment of cancer in older patients is not clearly defined, as oftentimes the elderly are excluded from clinical trials. Current treatment guidelines for older patients are proposed by cancer societies like the European Society for Medical Oncology (ESMO), the National Comprehensive Cancer Network (NCCN) and the International Society of Geriatric Oncology (SIOG).5,6
Over the past few years, precision medicine emerged as a key concept in cancer therapy, with tailored treatment becoming standard of care in many types of cancer. For example, more than 50% of lung adenocarcinomas, which is the most common type of lung cancer, harbor targetable mutations in the genes like EGFR, ROS1, RAS, BRAF, HER2, cMet and others.7 In this patient population with poor prognosis, new targeted drugs significantly improved clinical outcomes and quality of life. Notably, tailored treatment concepts are most relevant for older and frail patients suffering from cancer to prevent over-treatment and under-treatment.8,9 Moreover, immunotherapy and chemotherapy also need to be adjusted and their toxicity mitigated in the case of older oncologic patients. Oftentimes, due to comorbidities leading to immunosuppression, myelosuppression, anemia and infectious complications, standard chemotherapies are too risky for older cancer patients who cannot tolerate the toxicity associated with these regimens. Therefore geriatric oncologists tend to use immunotherapies to modulate the immune system and lower the risk for severe side effects and hospitalizations, apart from the seldom risk of autoimmune reactions.
Data showed that a multidisciplinary approach can improve communication between healthcare professionals, as well as between the healthcare professionals and patients.10 This can lead to a more coordinated and efficient healthcare plan, which can in turn improve patient outcomes. Indeed, studies demonstrated that a coordinated care plan is more likely to be followed and less likely to result in errors or missed appointments. A multidisciplinary approach can also help reduce the length of hospitalization and the need for hospital readmission.11 In addition, this concept is associated with increased patient satisfaction because patients are more likely to feel involved in their own care and treatment design when they can communicate openly with healthcare providers. The aim of the present study was to evaluate the level of experience and preferences among members of the interdisciplinary cancer diagnostic and treatment team regarding screening for frailty, decision tools and instruments.
Material and Methods
The Cancer Center Baselland in Switzerland was established in 2022 with the aim to provide care for cancer patients in the whole Canton Baselland with its 288,132 inhabitants. In this area, the number of patients with newly diagnosed cancer was 3,800 in 2022, accounting for around 8% of total Swiss cases.12 Before establishing the geriatric oncology unit, we sent a questionnaire to our multidisciplinary cancer care team, including oncologists, geriatricians, palliative care medicine physicians, dieticians, physical medicine physicians, psycho-oncologists, pharmacists, nurse practitioners, social service workers and spiritual care professionals. The questionnaire included questions about the professional team member and their experience in terms of geriatric oncology. The questionnaire was complied with a redcap database file and requested via email by each team member in the hospital. Each participant was asked to give feedback within four weeks. Furthermore, informed consent about analyzing and publishing data was obtained from each healthcare professional. The complete questionnaire in German can be found in Appendix 1 (https://cdn.healthbook.network/pim/2023/6/aca7a9ae-776f-4731-b6cc-5c34e6f647f9.pdf).
Results
This survey was used for the multidisciplinary team providing cancer care for patients, including older patients, in our oncologic center. We sent out 41 questionnaires and received 22 answers (54%) within four weeks. Figure 1 demonstrates the distribution of healthcare professionals. The most common participants were medical oncologists (n=3; 14%), followed by psycho-oncologists, social service workers, palliative care medicine physicians and spiritual care professionals (each n=2; 9%). In total, 9 male participants (44.9%) and thirteen female participants (55.1%) answered the questionnaire. Nearly all participants (95%) provided regular care for patients with cancer and all participants (100%) cared for geriatric patients. All participants were experienced healthcare professionals with a median of 20.45 years (range, 6−32) of experience in the field.
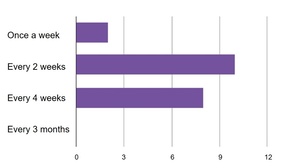
One important question regarded the frequency of having a multidisciplinary team meeting (MDT) of all professionals caring for older cancer patients, e.g., once a week, every other week or less frequent. Most participants voted for one meeting every other week (Figure 2). Another question was if an older patient with cancer will profit from such a regular MDT. The majority (n=20; 94.7%) of participants agreed that patients will have a clear benefit from regular MDTs. The next important question was the chronological age at which a standardized screening for frailty should be implemented. Most participants voted for the age of 70 years or older (76.2%), while 19% voted for 60 years or older, 4.8% for 80 years or older and 0% for 90 years or older.
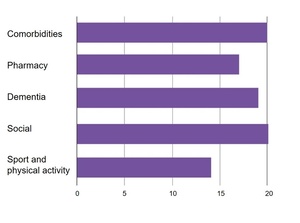
The next question was on the dimensions of screening and assessments in a geriatric oncology unit. There were the following topics to address: comorbidities, medication, dementia, social issues and physical activity. The most commonly selected dimensions were comorbidities and social issues (each n=20; 94.7%) (Figure 3).
Another important question was which specialist should be a part of the MDT for geriatric oncologic patients. The participants voted the following: geriatrician, oncologist (each n=20; 94.7%), advanced nurse specialist (n=18; 81.2%), palliative care physician (n=15; 68%), primary care physician (n=15; 68%), physiotherapist (n=14; 63.6%), psychiatrist (n=10; 45.5%), pharmacist (n=8; 36%), others (n=8; 36%), spiritual care professional (n=7; 31.8%), speech therapist (n=6; 27%) and internal medicine physician (n=5; 22.7%). So far, we have not sent the questionnaire to family doctors but we are considering their integration into this all-inclusive approach, since one of our co-authors is a family medicine specialist.
The next question assessed the knowledge of participants regarding the available frailty screening tools, including the Geriatric 8 (G8) score, Vulnerable Elders Survey-13 (VE13), Groningen Frailty Index (GFI), Triage risk screening tool (TRST), Edmonson Scale (EMED) Criteria, Barber test, abbreviated Comprehensive Geriatric Assessment (CGA) and Clinical Frailty Scale (CFS). The majority (n=12; 54.5%) voted for the G8 assessment score, which was also chosen as the preferred screening tool in our institution (n=12; 54.5%). Figures 4 and 5 illustrate these results.
Finally, the most common answers to the questions regarding recommended treatment optimization were the need to adjust for comorbidities (n=15; 68%) and optimize nutrition (n=15; 68%) prior to intervention and specific cancer treatment. The complete list of items is shown in Table 1.
Discussion
Switching healthcare focus to elderly cancer patients, with special attention on implementation of innovative technologies, is essential due to demographic changes resulting from the aging of the population and increasing life expectancy.13–16 Although more than 60% of cancer patients are older than 65 years,4 no clear guidelines exist on the implementation of care for older adults in the routine daily practice in Switzerland. On the other hand, there are several guidelines on special care for older patients, for example, NCCN guidelines, ESMO Guidelines and SIOG guidelines.5,6,17 Organ-specific guidelines for geriatric oncology also exist, for example, the recommendations regarding the management of older patients with breast cancer.18 In a recent review, we summarized current literature that addresses guidelines in geriatric oncology with a focus on palliative care in older patients with cancer19:
-
The nihilism in the field of palliative geronto-oncology is a major contributor to a reduced quality of life among the elderly with cancer and their families.
-
However, early palliative management of geriatric patients should always be aimed first at symptomatic treatment but potentially also at interventions and active anti-tumor therapies.
-
Especially in terms of the outcomes and improved quality of life for this specific population, with applicability not only for oncologists but for any involved physician, such as internists, palliative care and geriatric care specialists.
To our knowledge, there are only a few centers in Switzerland providing special geriatric oncology care or clinics dedicated entirely to older patients with cancer. In our center, more than 60% of patients with cancer are older than 65 years and the questionnaire therefore aimed to find a consensus on the optimal clinical care for these patients. As the canton Baselland has the second oldest population in Switzerland, there is a high need to assess current practices and optimize treatment and diagnostic approaches for this large patient population in the area. There are several questions in terms of optimal care for this population that need to be addressed for further healthcare planning. There is a challenge in terms of optimal ambulatory healthcare because of the travel distances and limited abilities of the elderly population in term of commuting. Further concepts including home care services needed to be considered and optimized. In our canton, we have a very dense network of general practitioners who provide regular check-ups to our patients and we believe they should be included when designing a comprehensive cancer care plan for older patients living in the area. Furthermore, the ambulatory nursing service including “Spitex” and “Onco-Spitex” need to be involved in further care planning.
On the other hand, optimized care planning should include relatives of patients, since they are oftentimes the main caregivers, especially in the case of older cancer patients. Relatives can help healthcare providers to determine the optimal needs of geriatric patients and can help patients with understanding and actively participating in designing of an optimal care plan.
Our approach includes a multidisciplinary team that cares for older patients with cancer. Most team members are experienced caregivers with an extensive working background and thorough knowledge in the field of geriatric oncology.
Conclusion and outlook
Systemically planned care for geriatric oncology patients is not an established practice in conventional healthcare centers in Switzerland. Our care team is experienced in caring for cancer patients, but we think more education is needed in order to bring the field of geriatric oncology forward in our hospital and also in Switzerland. In collaboration with international healthcare centers and groups, we plan to establish learning courses targeting healthcare providers, patients and their caregivers and we aim to set a foundation on which to start building new comprehensive practices and policies serving the needs of older cancer patients in Switzerland.
Conflict of Interest
Marcus Vetter received honoraria for consultancy from GSK, Roche, Novartis, Exact Sciences, Pfizer, Stemline, AbbVie and ASC Oncology. These funding entities did not play a role in the development of the manuscript and did not influence its content in any way. Other authors have declared that the manuscript was written in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Funding
All authors have declared that no financial support was received from any organization for the submitted work.
Author Contributions
All authors contributed to and approved the final manuscript.
Acknowledgments
We thank all participants who took part in this questionnaire.

.jpeg)
.jpeg)



.jpeg)
.jpeg)