Molecular subtypes defining risk of relapse
Until recently, endometrial cancer was defined by histology as either type I (endometrioid histology, obesity, hormone-receptor-positivity; usually good prognosis) or type II (mainly serous histology; bad prognosis) disease.2 This evolved to be insufficient to accurately estimate the risk of relapse in patients with endometrial cancer. Published in 2013, The Cancer Genome Atlas classification system was a breakthrough in the understanding of this disease.3 Molecular features in endometrial cancer have been acknowledged, which help to refine prognostic information. The primary goal of treating physicians is to improve the prognosis of patients and to apply personalized treatments.
De-escalating strategies are warranted where the prognosis is superior, e.g., in patients with polymerase epsilon (POLƐ)-mutated disease (Table 1).4 Those patients are likely over-treated by standard therapies since it is not fully clear whether this good prognosis is due to excellent treatment response or whether the course of the disease would be similar without treatment. On the other hand, tumors with a p53 dysfunction have a poor prognosis as a result of genomic instability and rapid progression.5
According to The Cancer Genome Atlas, four molecular classes with different prognoses are currently identified.3 The significant prognostic differences across the four subgroups were demonstrated in a retrospective analysis of the Post-Operative Radiation Therapy in Endometrial Carcinoma (PORTEC)-3 trial assessing the benefit of combined adjuvant chemotherapy and radiotherapy versus radiotherapy alone in women with high-risk endometrial cancer.5,6 In this study, molecular testing of 410 tumors revealed the following distribution of molecular subtypes: 33.4% had mismatch repair deficiency (dMMR), 31.5% had non-specific molecular profile (NSMP), 22.7% were p53 abnormal and 12.4% were POLƐ-ultramutated. Data further indicated an excellent prognosis in patients with POLƐ-mutated tumors, including those with histologically aggressive features (Figure 1).5 For poorly differentiated tumors (grade 3), 12% had POLƐ-mutations, 40% had dMMR, 18% had a p53 mutation and 30% had NSMP in all carcinomas.7
New risk definition by molecular subtypes in upcoming clinical trials
In 2021, new guidelines for the treatment of endometrial cancer were published by the European Society of Gynecological Oncology (ESGO), the European Society of Radio-Oncology (ESTRO) and the European Society of Pathology (ESP).8 These recommendations integrate the new risk definition by molecular (prognostic) features, which are of extreme importance in paving the way to personalized medicine.
To date, there are no robust data on the predictive value of results from clinical trials in endometrial cancer, as only data from retrospective studies are available. For example, a retrospective analysis of the PORTEC-3 trial showed no evidence of a benefit of adding chemotherapy to radiotherapy in a small group of dMMR patients.5 These data have to be corroborated in prospective randomized trials, such as the ongoing phase III PORTEC-4a trial (ClinicalTrials.gov Identifier: NCT03469674).9 In this international, randomized, prospective trial, patients with high-intermediate risk endometrial cancer will be randomized 2:1 to receive either an individual (experimental) treatment, based on molecular subtypes, or standard treatment. After surgery, patients will either be cared for with watchful waiting without any therapy (favorable risk), or receive brachytherapy (intermediate risk), or external beam radiation therapy (EBRT) (unfavorable risk). Patients from Switzerland will also be included in this study.
Furthermore, molecular insights from the PORTEC-3 trial will be investigated in the comprehensive international project Refining Adjuvant treatment IN endometrial cancer Based On molecular features (RAINBO), TransPORTEC platform trials. Molecular risk stratification and biological features are implemented to personalize adjuvant therapy (Table 1). This project will commence internationally in early 2022. In Switzerland, participation will be through our national cooperative investigating group, the Swiss Group for Clinical Cancer Research (SAKK). These results are eagerly anticipated as they can offer enormous possibilities for precision medicine.
How to approach metastatic disease?
The following pathological biomarkers are required to decide on adequate treatment:
-
Estrogen receptor (ER)
-
Progesterone receptor (PgR)
-
Human epidermal growth factor receptor (HER) 2-status in serous endometrial carcinoma
-
MMR proteins (MLH1, PMS2, MSH2, MSH6), programmed death-ligand 1 (PD-L1)
-
Microsatellite instability (MSI), tumor molecular burden (TMB)
About 3% of endometrial or colorectal cancers are caused by Lynch syndrome, formerly named hereditary non-polyposis colorectal carcinoma (HNPCC), which is due to mutations in DNA mismatch repair genes, including MLHL, MH2, MSH6, PMS2 and EPCAM.10 In universal tumor screening recommended by the National Comprehensive Cancer Network (NCCN) guidelines, patients with endometrial or colorectal cancer should be tested at primary diagnosis for dMMR by immuno-histochemistry in the MLH1, PMS2, MSH2 and MSH6 genes.11 Tumors with a loss of expression (dMMR) and without MLH1 promoter hypermethylation should be further investigated for MSI. Should a relevant family history of Lynch syndrome-associated tumors be revealed, patients are also offered genetic counseling. MSI should be considered even for patients without dMMR. In the case of MSI-high (MSI-H), germline testing is recommended to clarify the presence of Lynch syndrome.
In the metastatic setting, patients with tumors overexpressing PD-L1 should be considered for therapy with ICIs. Both, MSI-H and high TMB are predictive biomarkers of immunotherapy response.12 A further important immuno-histochemical parameter is the L1 cell adhesion molecule (L1CAM). Its overexpression has been shown to be of significant prognostic importance,13 however predictive approaches are still lacking. In the future, a combination of histopathological features (lymphovascular space invasion [LVSI], L1CAM) and new molecular subtypes will have the highest prognostic impact.
First-line treatment of endometrial cancer
Palliative endocrine therapy
Patients with tumors with low-grade histology, ER-positivity and slow disease progression seem to benefit most from endocrine treatment (ET).14 ET often leads to long-lasting disease control with relatively few side effects. Over half of the patients in this setting may achieve prolonged responses to progestogens (medroxyprogesterone-acetate [200–300 mg] and megestrol-acetate [160 mg daily] are recommended). In terms of safety, there is an elevated risk of thromboembolic events, as well as a significant increase in weight.15 ET can also be recommended for patients with hormone-receptor (HR)-negative disease.14
Several trials aimed to intensify the efficacy of endocrine monotherapies, for example, by combining an aromatase inhibitor (AI) with a mTOR inhibitor such as everolimus. However, in elderly patients, the toxicity profile of everolimus must be considered (e.g., mucositis, interstitial lung disease).16 At the European Society for Medical Oncology (ESMO) Congress 2020, phase II data were presented on the combination of the AI letrozole and the CDK4/6-inhibitor palbociclib, showing a clinically meaningful improvement of progression-free survival (PFS) with this treatment regimen in patients with advanced or recurrent ER-positive endometrial cancer.17 These data should be confirmed in a phase III trial.
Palliative chemotherapy
Originally, the first-line chemotherapy for the treatment of endometrial cancer was anthracycline-based. Doxorubicin is an anthracycline that has been investigated as monotherapy and in combination with cyclophosphamide and cisplatin in this patient population.18 In the GOG-209 trial, the combination chemotherapy of paclitaxel, doxorubicin and cisplatin (TAP) versus carboplatin and paclitaxel (CP) was assessed in nearly 1,400 patients with metastatic endometrial cancer.19 The doublet CP demonstrated a favorable safety profile, with non-inferiority in terms of overall survival (OS). Thus, CP remains the standard of care in this clinical setting.
Combining carboplatin and paclitaxel with the monoclonal antibody bevacizumab, a vascular endothelial growth factor (VEGF) inhibitor, led to non-significant improvement in PFS and OS outcomes in patients with advanced or recurrent endometrial cancer in the randomized, phase II MITO END-2 trial.20 This combination regimen has not yet been approved by the Food and Drug Administration (FDA).
Second-line treatment of endometrial cancer
Before the era of immunotherapy, there was no standard treatment in the second-line therapy for patients with endometrial cancer. After disease progression, treatment with subsequent chemotherapies was often not successful, response rates around 10% with anthracyclines were disappointing and platinum- and taxane-free regimens showed little benefit.19 Among patients with an adequate time interval (>24 months) after the last platinum-based chemotherapy, re-challenge with platinum achieved response rates of more than 60%.21 However, treating patients in a clinical trial was (and still is) the best option.
To date, different programmed cell death protein 1 (PD-1) and PD-L1 inhibitors have been developed for the treatment of relapsed endometrial cancer. PD-1 is an immune checkpoint protein that is expressed by tumor-infiltrating lymphocytes. When activated by PD-L1, T-cell activity is blocked and immune-evasion is promoted. In the case of dMMR, tumors are especially sensitive to anti-PD-1/PD-L1 antibodies.22 Immunotherapy is generally well tolerated and immune-related side effects are mostly mild. As patients with endometrial cancer are often older and frail, it is essential to consider all comorbidities.23 The most prevalent side effects of ICIs are pruritus, rash, fatigue, diarrhea, nausea, loss of appetite, fever, cough, dyspnea and musculoskeletal pain. Immune-related toxicity such as pneumonitis, colitis, hepatitis, endocrinopathies and nephritis are rare. However, as they are associated with potentially great harm, it is key to recognize them early. Fortunately, patients can often benefit from long durations of responses.
In 2017, pembrolizumab, a PD-1 inhibitor, was approved by the FDA as the first tumor-agnostic molecule, based on the phase II KEYNOTE-028 trial on solid tumors with MSI-H/dMMR after progression on standard treatment.24 The efficacy of pembrolizumab in endometrial cancer was confirmed in the phase II KEYNOTE-158 trial, with 70% of patients experiencing a tumor size reduction of ≥30%.25
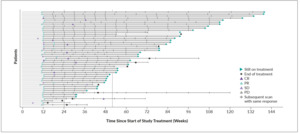
In 2020, Makker et al. published results from a phase Ib/II study assessing the efficacy of pembrolizumab in combination with lenvatinib, an oral VEGF receptor 1−3 inhibitor, in patients with advanced endometrial cancer.26 At baseline, nearly all patients (87%) were microsatellite stable (MSS) or MMR proficient (pMMR) and a PD-L1-positivity was observed in 50% of patients. The overall response rate (ORR) was relatively high at 36%, considering the pre-treatments of these patients. In patients with evaluable tumor assessments by investigators per immune-related response evaluation criteria in solid tumors (irRECIST) (n=102), the sum of diameters of target lesions decreased from baseline in 84.3% of patients (Figure 2). In about 40% of patients, long-lasting responses were achieved. Clinical benefit was also seen in difficult-to-treat histologies such as serous endometrial cancers. Regarding safety, treatment-related side effects were considerable, with grade 3–4 toxicity occurring in about 70% of patients and mainly included nausea, diarrhea, hypertension and fatigue. Dose modifications were necessary for 70% of patients. Based on these data, pembrolizumab plus lenvatinib was approved by FDA in 2021 for the treatment of patients with advanced endometrial carcinoma that is not MSI-H or dMMR and who have disease progression following prior systemic therapy.27
Oaknin et al. (2020) presented encouraging data from a single-arm phase I trial (GARNET) on dostarlimab, another anti-PD-1 antibody, in patients with recurrent or advanced dMMR endometrial cancer.28 An update of the study reported during ESGO Congress 2021 included data from two expansion cohorts of patients with dMMR (n=129) and pMMR (n=161).29 At data cutoff, the ORR was 43.3% in the dMMR group and 13.4% in the pMMR group, with a median duration of response (DOR) not reached in both groups. More than 90% of the responding patients remained in response ≥6 months (range: 2.6–22.4 months, ongoing on last assessment) (Figure 3). Treatment was well tolerated, with a toxicity profile as expected with ICIs. FDA approval of dostarlimab in this patient population followed in 2021 due to these promising results.30 In February 2022, Swissmedic approved dostarlimab for the treatment of adult patients with dMMR recurrent or advanced endometrial cancer that has progressed on or following a prior platinum-containing regimen.31 The approval is based on results from the dMMR endometrial cancer cohort of the GARNET study, in which dostarlimab showed an ORR of 42.3% in 71 patients with dMMR recurrent or advanced endometrial cancer.32 This included a complete response (CR) rate of 12.7% and a partial response (PR) rate of 29.6%.
In Switzerland, pembrolizumab is approved as monotherapy for the treatment of patients with metastatic endometrial cancer with MSI-H or dMMR who have progressed after standard therapy and for whom no satisfactory treatment alternatives are available.33 Swissmedic approval is awaited this year for pembrolizumab plus lenvatinib in pMMR endometrial cancer patients.
The story of immunotherapy in endometrial cancer goes on
There are several ongoing trials of combination therapies with immunotherapy in patients with endometrial cancer. For example, the Italian phase III AtTEnd trial (NCT03603184) is currently investigating atezolizumab, a PD-L1 inhibitor, in combination with carboplatin and paclitaxel in women with advanced/recurrent endometrial cancer, independent of MMR status.34 Furthermore, the phase III KEYNOTE-775 trial (NCT03517449) aimed to assess pembrolizumab in combination with lenvatinib versus doxorubicin or paclitaxel in patients with advanced endometrial cancer.35 Dostarlimab is being evaluated in the phase III trial (NCT03981796; RUBY) in combination with carboplatin/paclitaxel in patients with recurrent or primary advanced endometrial cancer.36
Immunotherapy in combination with poly-ADP-ribose-polymerase (PARP) inhibitors, antiangiogenic molecules or radiotherapy also emerged as a promising treatment strategy in patients with endometrial cancer.37–39 All these combination therapies are currently being investigated in clinical trials, offering hope for more well-tolerated treatment options.
Conclusions
-
Early-stage endometrial cancer is the most common gynecological tumor in Europe and the US, usually with an excellent prognosis.
-
Integrated as risk factors in the new ESGO-ESTRO-ESP guidelines 2021, molecular biomarkers should be tested in all patients with endometrial cancer.
-
Metastatic endometrial cancer is treated with palliative endocrine or platinum-based chemotherapy regimens in the first line.
-
There are new second-line treatment options with immune checkpoint inhibitors (ICIs), such as pembrolizumab and dostarlimab for deficient mismatch repair (dMMR) endometrial cancer, as well as the combination of pembrolizumab and lenvatinib for MMR-proficient (pMMR) endometrial cancer.
Conflicts of Interest
Consultancy for AstraZeneca, GSK and Merck
Author Contributions
The author crafted and approved the final manuscript.
_by_molecular_subtypes_in_endometrial_cancer.**_abn__aberr.jpg)
_by_microsa.png)
_by_molecular_subtypes_in_endometrial_cancer.**_abn__aberr.jpg)
_by_microsa.png)
